
It is not rocket science to work out that healthcare settings are potentially dangerous places where Covid and other viruses can spread. Over the course of the pandemic measures aimed at making healthcare safe have been removed with the result that many clinically vulnerable families avoid attending healthcare settings in person. This blog discusses some of the recent development and campaigns and will be updated.
To recap, the reasons why healthcare settings are potentially dangerous to clinically vulnerable people and more generally include:
– patients and visitors are more likely to be clinically vulnerable or elderly compared with the general population.
– People who are ill with symptoms (which may or may not be Covid) tend to attend doctors surgeries or hospitals; and
– Healthcare workers are more likely to come into contact with Covid in their day to day work compared to the general population, and also have the potential to spread the virus.
Efforts made to protect patients and staff have evolved throughout the pandemic . Although healthcare settings, including hospitals, do not generally have the levels of ventilation needed to combat airborne infections, there is some anecdotal evidence that efforts were made to open windows, at least some of the time, in 2020 and 2021. During this period it was also a requirement to wear a face covering in a healthcare setting. This usually meant baggy blue type surgical masks (as in the photo above) which as explained in my blog on Avoiding Covid are relatively weak in protecting against the particular airborne nature of Covid, but at least they were providing some protection if everyone was wearing one. Healthcare workers were also required to regularly test for the virus and required to isolate if they tested positive.
However, requirements to wear a mask and other mitigations including testing and isolation, have been systematically dismantled since the spring of 2022 as part of the general strategy of ‘living with Covid’. This began with specifying where mask wearing was still required towards the general free for all, with a few individual exceptions that has existed until recently.
Consequences of dismantling protections in healthcare
The consequences of this dismantling for vulnerable patients, for staff and for everyone attending healthcare are potentially very serious. It is worth considering that many clinically vulnerable patients will not have responded to vaccination and are unprotected. Yet healthcare is the one place they really need to attend to manage their respective illnesses. A recent study from Wales estimated that over half of all Covid infections originated from attended hospitals.
As a consequence there is very significant anecdotal evidence that clinically vulnerable patients have been withdrawing from attending healthcare settings for fear of catching Covid, which could after all kill them. This is certainly true of my household where we avoided attending A and E on one occasion and as it happens, successfully managed the condition ourselves with the help of emergency drugs prescribed via a 111 doctor.
Survey evidence supports this. A recent survey found that half of clinically vulnerable people had cancelled a medical appointment over concerns about lack of Covid precautions and more than a quarter had cancelled or declined a vaccine booster for the same reason. Other surveys have found that the vast majority of clinically vulnerable people and their families are uncomfortable with attending healthcare even if they go ahead and attend.
Government Petition calling for a return of masks in healthcare
In a desperate attempt to get the government to stand up and take notice the Clinically Vulnerable Families group launched a petition in May 2023 with the following wording.
‘We urge the Government to implement a policy requiring mask wearing in all healthcare settings including hospitals, clinics and GP practices for staff, visitors and patients. An FFP2 minimum should be mandated, to protect against infectious diseases, including COVID-19’.
As those familiar with government petitions will know 10,000 signatures are required to trigger a response from government and 100,000 are required to be considered for a parliamentary debate.
After an initial spurt of enthusiasm in which several thousand signatures were collected in the first few days, getting to 10,000 proved to be quite an effort against a wall of indifference for those like myself working hard to promote it. We did achieve this with time to spare, achieving 10,531 signatures before the 12 October deadline.
We were, however, rewarded with an outrageous response from the government which simply reiterated the same old position.It did not acknowledge the problems being caused, including for clinically vulnerable families at all.
‘The current guidance for face masks and Personal Protective Equipment allows for a risk-based approach. It provides guidance on how providers can ensure that measures put in place are effective, proportionate and appropriate to protect those most at risk of severe outcomes from respiratory infections. UKHSA and NHSE continuously monitor COVID-19 infection rates amongst healthcare workers in England and review, update and publish appropriate guidance based on the scientific evidence.’
However, and rather unusually, the 11 member parliamentary cross bench ‘petitions committee’ batted the response back to the government for redrafting. We await the government redraft in hope, if not expectation.
‘The Petitions Committee (the group of MPs who oversee the petitions system) have considered the Government’s response to this petition. They felt that the response did not directly address the request of petition and have therefore written back to the Government to ask them to provide a revised response’.
Signs of Change
In recent weeks there have been a few hopeful signs of a change in attitude amongst healthcare providers. Sheffield Hospitals have reintroduced a requirement to wear a mask due to the significant rise in cases. It is also clear that a few other hospitals and healthcare settings are reintroducing masks and more generally, an increasing minority of staff and patients/visitors are wearing a mask on their own initiative.
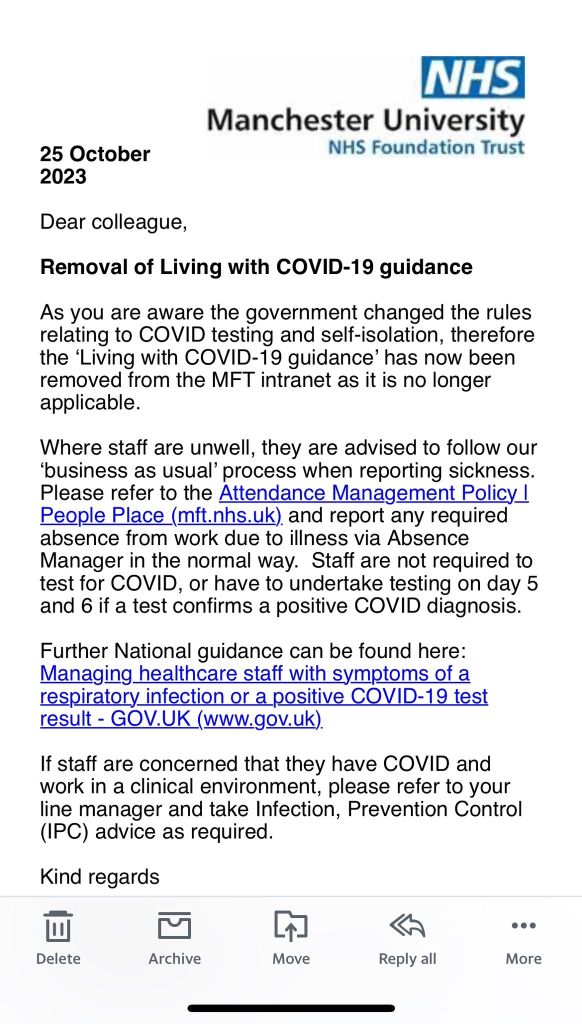
However, these good examples are in the minority at the moment. In sharp contrast, in Manchester health authority have taken it upon themselves to almost discourage staff testing for Covid and have implemented a sick leave policy in line with any other staff illness. This completely ignores the highly transmissibility of Covid via the air and the fact that unlike flu type droplets it can hang about in the air for hours.
It is not at all clear how this is going to play out as we approach the winter. The hope is that the government comes under pressure and changes the central guidance on safety in healthcare settings, including the wearing of good quality masks. However, it is more likely that change will be driven from local health providers who realise that they need to improve safety for staff if they are to avoid NHS healthcare falling apart this winter due to high staff absences and high rates of infection.
Government responds to petitions committee
The Government’s response to the petitions committee request that the original government response be revised has been received. The words have been shuffled around somewhat but otherwise there is no change.
The response fails to address the evidence that clinically vulnerable people and their families are avoiding attending healthcare because of the dangers.
The response also implies that the situation is constantly reviewed. Yet we know that this is not the case. There are no national guidelines on testing air quality in clinical settings and testing of patients has dropped dramatically so we have no idea how dangerous or otherwise healthcare settings are. Moreover, staff no longer have access to free tests so we do not know the rate of infection amongst NHS staff.
This is very disappointing and makes a mockery of parliamentary processes. As noted above, it seems that the only way we are going to make progress in the short term is to lobby at the local level. I am personally involved in doing this as are many other people.
Leave a comment